CDC investigating botched Botox shots in 9 states
-

Dartmouth researchers look to meld therapy apps with modern AI
Therabot, currently in its first clinical trial, uses generative AI trained on therapy scripts in an effort to create technology that brings mental health services to underserved populations.
-

Houston hospital says doctor made patients ineligible for liver transplants by manipulating database
A Houston hospital has halted its liver and kidney transplant programs after it says a doctor manipulated a database for liver transplant patients, making them ineligible to receive a new organ.... -

As bird flu spreads in the US, is it safe to eat eggs? What to know about the risk to humans
Bird flu has spread to dairy cows in multiple states and one person in Texas. Here’s what to know about transmission, symptoms and food risks.
-
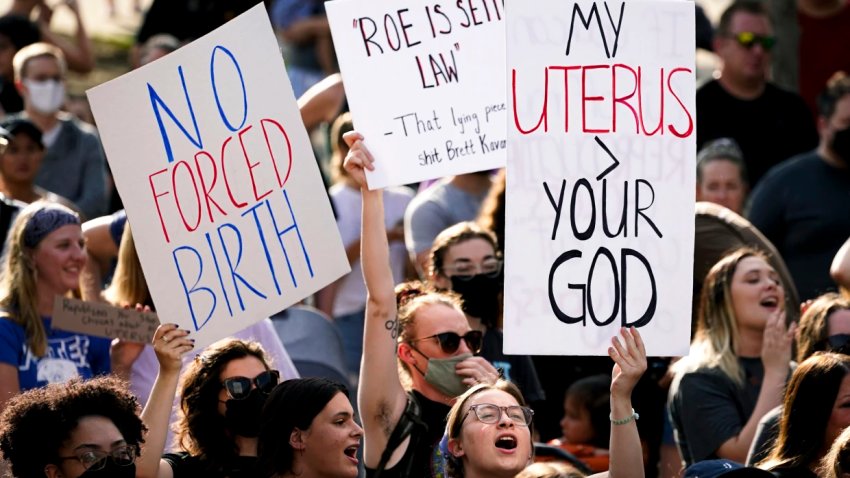
More young people choosing permanent sterilization after abortion restrictions
Since the Supreme Court overturned Roe v. Wade, there’s been an ongoing increase in adults ages 18 to 30 who undergo tubal ligation or vasectomy, new research shows.